Implementation of
Digital Health and Precision Medicine
INCASYM (Integrated Care and Systems Medicine) is a collaborative platform of multidisciplinary professionals, originated at Barcelona Clínic Ecosystem, networking with other health-related institutions such as The Digitalization for Health System Sustainability (DS3) group of the Catalan Department of Health and the European joint action Jadecare (www.jadecare.eu).


Our Vision
Revolutionizing healthcare by introducing a more efficient and patient-centric system that benefits both healthcare providers and citizens.
Our Mission
Driving collaborative research and innovation to develop evidence-based services designed to deliver patient-centered care.
Digital Health and AI Tools
Offering cost-effective services designed to provide personalized care and improve patient outcomes, emphasizing shared decision-making along the patient journey.
Leveraging advanced technologies to support early diagnosis, risk assessment, adaptive case management and patient empowerment for self-management.
Integrated Care Services
Promoting proactive prevention strategies for healthcare value generation and enhanced quality of life.
Focus on Prevention
Research and Innovation
The conceptual and strategic ap proach is described in the chapter Multilevel Modelling with AI: The Synergy-COPD Endeavour in the book Personalized Medicine meets Artificial Intelligence (2023), and in the doctoral thesis of Rubén González Colom: Predictive Modelling for Personalised Multimorbidity Management (January 2024).
The INCASyM group has two main areas of interest:
- Population HRA: Validation and support for the transfer/adoption of population risk stratification tools at EU level, through implementation science methodologies.
- Clinical HRA: Development of predictive computational models of individual risk that integrate data from various health determinants from different levels of care: 1) Data from the health system (medical records), 2) Capture of patient information (sensors and/or questionnaires), 3) Expressive omics data from endotypes; and 4) Data from population registers.
Our goal is to develop this line by facilitating the convergence of these two areas, in accordance with the conclusions of the expert meeting: Integrating Care, Strengthening Communities: The Data Connection (May 2024).
RISK PREDICTION MODELLING
APPLICABILITY AT THE POPULATION LEVEL AND IN THE CLINICAL FIELD
TOWARDS A MATURE DIGITAL TRANSFORMATION
While the potential of digital health is recognized in terms of improving the quality, safety, effectiveness, and efficiency of well-established healthcare processes, its large-scale adoption is still insufficient and immature, especially when digital transformation involves process reengineering and change management.
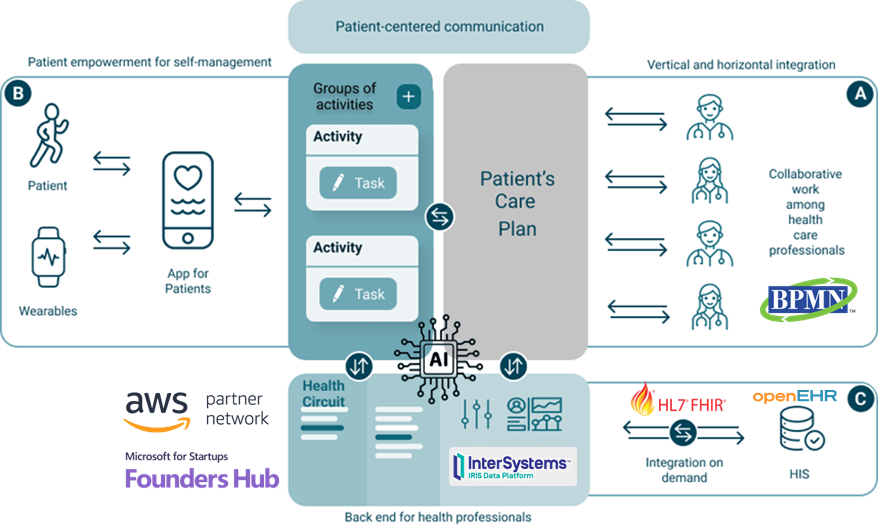
In this scenario, in addition to the common need for interoperability with existing electronic medical records, digital health tools must be easily adaptable to the objectives of health services, the requirements of health professionals and, of course, the needs of patients. It is necessary for healthcare professionals to have the ability to drive digital transformation by personalizing digital health tools, without requiring technical skills, in terms of clinical content and workflows, depending on the objectives of the healthcare service, the degree of standardization of processes and the changing needs of their target patients.
To this end, INCASYM has engineered the Health-Circuit's adaptive case management (ACM) platform to advance in the current state of the art in process automation based on the BPMN 2.0 standard to enable collaborative clinical processes, involving health professionals from different levels of care (A) and the patient himself (B), and that require flexibility to adjust the work plan dynamically according to unplanned health events and the evolution of each patient.
Health Circuit adopts a Cloud Native and Zero Trust architecture for easily scalable and highly secure deployment as a Software as a Service (SaaS) in various healthcare environments (C).
Implementation
The first large randomized controlled trial carried out in the UK (2011) showed that monitoring with telemedicine solutions for the management of chronic patients presented significant problems in terms of generating efficiencies in health systems.
Over the last decade, several relevant studies on the modulating factors of the scalability of integrated care services with digital support have made it possible to acquire a certain maturity in terms of the factors and methodologies that must be taken into account for the success of the digital transformation of the health field, beyond integrated care. As a result of this knowledge, the areas of work and objectives that we propose, based on the results of the last three doctoral theses on the subject, are described below. It should be mentioned that the team's activity focuses on any type of health service with proven effectiveness, not just integrated care.
Areas of work:
- Modelling of clinical processes managed by professionals from different providers and/or levels of care: support for clinical decisions, collaborative work, data capture, accessibility and empowerment of patients, etc. The conceptual and technical approach is described in Herranz C.
- Methods to optimize the deployment, scalability and transferability of value-generating health services (efficiencies). Reducing the gap between efficacy and effectiveness.
- Applicability of health services evaluation tools with a "Fivefold Aim" approach and the evaluation of the deployment of healthcare services. Tools for maintaining post-adoption quality.
- Clinical applicability of risk prediction (AI) tools in the clinical field.
DEPLOYMENT/SCALABILITY OF HEALTH SERVICES
WITH DIGITAL SUPPORT
+10
International Projects
+50
Active Collaborators
+80
Scientific Publications
Selection of the most recent publications
2024
Gezsi A et al. Unique genetic and risk-factor profiles in clusters of major depressive disorder-related multimorbidity trajectories. Nat Commun. 2024 Aug 21;15(1):7190. doi: 10.1038/s41467-024-51467-7. PMID: 39168988; PMCID: PMC11339304.
Gonzalez-Colom R et al. Toward Adoption of Health Risk Assessment in Population-Based and Clinical Scenarios: Lessons From JADECARE. Int J Integr Care. 2024 Jun 4;24(2):23. doi: 10.5334/ijic.7701. PMID: 38855028; PMCID: PMC11160407.
González-Colom R et al. Multicentric Assessment of a Multimorbidity-Adjusted Disability Score to Stratify Depression-Related Risks Using Temporal Disease Maps: Instrument Validation Study. J Med Internet Res. 2024 Jun 24;26. doi: 10.2196/53162. PMID: 38913991; PMCID: PMC11231623.
Folguera, J., et al. Retrospective analysis of hospitalization costs using two payment systems: the diagnosis related groups (DRG) and the Queralt system, a newly developed case-mix tool for hospitalized patients. Health Econ Rev 14, 45 (2024). https://doi.org/10.1186/s13561-024-00522-6
Hernandez C et al. The Value of Admission Avoidance: Cost-Consequence Analysis of One-Year Activity in a Consolidated Service. Cost Eff Resour Alloc. 2024 Apr 15;22(1):30. doi: 10.1186/s12962-024-00536-1.
González-Colom R et al. Five years of Hospital at Home adoption in Catalonia: impact, challenges, and proposals for quality assurance. BMC Health Serv Res. 2024 Feb 1;24(1):154. doi: 10.1186/s12913-024-10603-1. PMID: 38297234; PMCID: PMC10832077.
Herranz C et al. Toward Sustainable Adoption of Integrated Care for Prevention of Unplanned Hospitalizations: A Qualitative Analysis. Int J Integr Care. 2024 Jun 28;24(2):28. doi: 10.5334/ijic.7724. PMID: 38948163; PMCID: PMC11212778.
2023
González-Colom R et al. Prevention of Unplanned Hospital Admissions in Multimorbid Patients Using Computational Modeling: Observational Retrospective Cohort Study. J Med Internet Res. 2023 Feb 16;25. doi: 10.2196/40846. PMID: 36795471.
Cano et al. Multilevel Modelling with AI: The Synergy-COPD Endeavour. In: Personalized Medicine meets Artificial Intelligence (a Cesario, M D’Oria, Ch Auffray and G Scambia eds), 2023, chapter 10; pp 131-144. Publisher: Springer Nature Switzerland AG 2023 https://doi.org/10.1007/978-3-031-32614-1
Risco R et al. Actionable Factors Fostering Health Value Generation and Scalability of Prehabilitation: A Prospective Cohort Study. Ann Surg. 2023 Aug 1;278(2). doi: 10.1097/SLA.0000000000005662. Epub 2022 Aug 15. PMID: 35968894; PMCID: PMC10321511.
Herranz C et al. A Practice-Proven Adaptive Case Management Approach for Innovative Health Care Services (Health Circuit): Cluster Randomized Clinical Pilot and Descriptive Observational Study. J Med Internet Res. 2023 Jun 14;25. doi: 10.2196/47672.
OECD (2023), Catalan Hospital at Home Program 2015-2019. Integrating Care to Prevent and Manage Chronic Diseases: Best Practices in Public Health, OECD Publishing, Paris, https://doi.org/10.1787/9acc1b1d-en.
OECD (2023), BSA integrated care services. Integrating Care to Prevent and Manage Chronic Diseases: Best Practices in Public Health, OECD Publishing, Paris, https://doi.org/10.1787/9acc1b1d-en.
OECD (2023), Prehabilitation Case Study. OECD Best Practices (https://www.clinicbarcelona.org/en/news/the-surgifittm-digital-platform-is-recognized-as-a-good-practice-for-strengthening-public-health-systems)
2022
Baltaxe E et al. Role of co-creation for large-scale sustainable adoption of digitally supported integrated care: prehabilitation as use case. Int Journal Integrated Care. 2022. 22(4): 1, 1–12. https://doi.org/10.5334/ijic.6503
Herranz C et al. Prospective cohort study for assessment of integrated care with a triple aim approach: hospital at home as use case. BMC Health Serv Res. 2022 Sep 7;22(1):1133. doi: 10.1186/s12913-022-08496-z.
Baltaxe E et al. Assessment of digital tools supporting healthcare services for chronic patients: experience from a dual hospital. J Med Internet Res. 2022. https://www.doi.org/10.2196/40976
Doctoral Thesis
An Adaptative Case Management Approach to Prevent Unplanned Hospital Admissions in a Care Continuum Scenario. Carme Herranz Nurse (Barcelona). Defense at University of Barcelona, on 12th December 2023.
Predictive Modelling for Personalized Multimorbidity Management. Rubèn Gonzalez-Colom Biologist & Data Scientist (Barcelona). Defense at University of Barcelona on 29th January 2024. (http://hdl.handle.net/10803/691632)
Evaluation and digital transformation of integrated care services. Erik Baltaxe MD (Israel) Defense at University of Barcelona. 3rd July 2024.
Contact
©Derechos de autor. Todos los derechos reservados.
Necesitamos su consentimiento para cargar las traducciones
Utilizamos un servicio de terceros para traducir el contenido del sitio web que puede recopilar datos sobre su actividad. Por favor revise los detalles en la política de privacidad y acepte el servicio para ver las traducciones.
